Gum disease incorporates both gingivitis and periodontitis with symptoms that can range from inflammation indicated by slight redness of the gums to gum recession, severe infections, and tooth loss. Gingivitis is an inflammation of the gums, which can lead to periodontitis if left untreated. Regular visits to the dentist will help catch and treat any signs of gum disease early so that it does not progress into periodontitis, and good oral hygiene practices can also help prevent the onset of periodontal disease. But life happens, and if you do find yourself with more advanced forms of gum disease, be sure to contact your dentist as soon as possible for evaluation and treatment.


Periodontal Disease Stages & symptoms
Symptoms of the onset of periodontal disease can often be mild and therefore go unnoticed. However, left untreated, this can lead to some serious dental, and even general health problems. The periodontal disease stages and symptoms are outlined below, so if you experience any of these, please contact your dentist for immediate evaluation and treatment.
gingivitis (inflamation)
Inflammation of the gums is one of the first signs of gum disease, often indicated by bleeding when brushing or flossing. You may also notice some redness and swelling, but usually little or no discomfort or pain. This early stage is called gingivitis, and when caught at this stage, professional treatment by a dentist combined with good oral hygiene can reverse the condition.
early periodontal disease
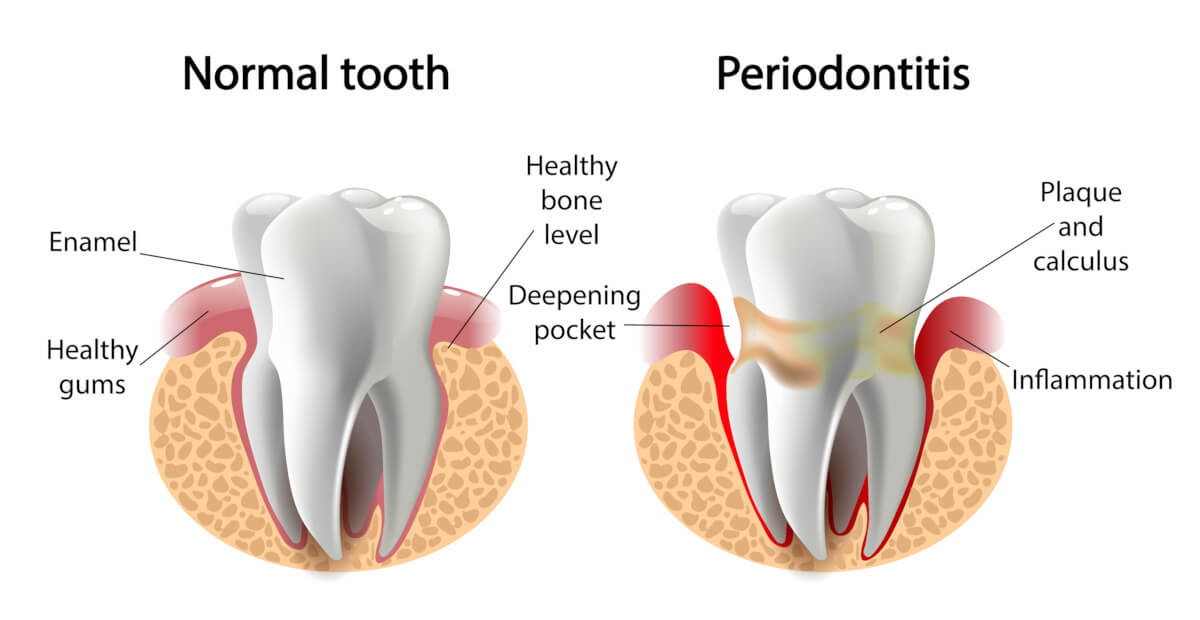
When gingivitis is left untreated, buildup of plaque may spread and begin to grow below the gum line. This causes the gums to recede away from the base of the tooth to form pockets that can harbor the growth of harmful bacteria. At this stage, you may notice a “lengthening” of the tooth where the root is exposed due to gum recession, and there may be some sensitivity.
moderate periodontal disease
At the moderate stage, you may begin to experience some pain and increased bleeding around the area of the gum recession. As the gum continues to recede and bacteria continues to grow, toxins are released that may break down the bone and tissue that hold teeth in place, resulting in the affected tooth becoming loose.
advanced periodontal disease
In advanced periodontal disease, the gums, bones, and connective tissues that support the teeth and hold them in place are broken down and destroyed. Pain becomes more pronounced at this stage, especially when chewing, and you may experience a foul taste in your mouth along with bad breath. Once periodontal disease reaches this point, there is a high chance of significant tooth loss.
gum disease symptoms
In summary, there are a range of gum disease symptoms to look out for throughout its stages of development. These begin with slight bleeding when brushing or flossing with a little swelling and redness and can develop to bad breath, gum recession, plaque buildup, and loose teeth. Discomfort and pain gradually increase as the disease progresses and foul taste and tooth loss with inflammatory responses throughout the body may be experienced at the advanced stages. If you experience any of these symptoms, however mild, it is important to contact your dentist immediately for evaluation and treatment to prevent further progression of the disease.
Gum Disease treatment
There are a variety of methods of gum disease treatment depending on the severity of case and symptoms ranging from deep cleaning procedures to surgery. The most common treatments and procedures are outlined below.
For patients in the early phases – usually at the gingivitis stage – a specific method of deep cleaning called periodontal scaling followed by root planing may be sufficient to restore gum health. Periodontal scaling is a technique where plaque and tartar are carefully removed from the surface of your teeth, including from below the gum line, whereas root planing involves removal of plaque and tartar from the root surfaces.
gum surgery
Sometimes the periodontal pockets deepen to a point that makes periodontal scaling difficult and daily maintenance ineffective. In this case, gum surgery may be required. In this procedure, also called flap surgery or pocket reduction surgery, incisions are made in the gums to flap back the tissue for effective deep cleaning. The gums are then reattached to fit snugly around the tooth to reduce the gap between the gum and teeth.
gum graft
Gum, or soft tissue grafts may be performed when receding gums are an issue. The soft tissue graft involves taking gum tissue from elsewhere in the mouth (most often from the root of the mouth) and adding the tissue to the affected area to restore thin or receding gums.
regenerative procedures
Advanced periodontal disease causes destruction to the bone that supports the teeth. In this case, a bone graft may be required to encourage regeneration of the bone and restore stability to the affected tooth. Often at this stage, tooth loss has already occurred, and patients may be candidates for dental implant surgery if adequate bone has been regenerated.
If periodontal disease has advanced to a point where the natural teeth cannot be saved, tooth extraction may be necessary. Depending on the condition of the supporting bone, dental implant surgery may be possible to restore functionality and an even smile.
Get a consultation from our dentist in Aurora, CO. Call us to make an appointment today!
FAQs on Periodontal disease
how can gum disease be prevented?
The best treatment for gum disease, as with any health condition, is prevention. Even if you show signs of gingivitis or early gum disease, quick action and ongoing maintenance can help prevent further progression of the disease and even reverse it. The control of plaque is key to the prevention of periodontitis, and this can be maintained with bi-annual professional teeth cleaning by a dentist combined with good general oral hygiene practices. Some factors that may contribute to the risk of periodontitis include smoking, stress, poor nutrition, teeth grinding, certain medications, having a dry mouth, as well as genetic predisposition.
How do I practice good oral hygiene for prevention of periodontitis?
Good oral hygiene practices consist mainly of brushing and flossing. Teeth should be brushed at least twice a day for two minutes, once in the morning and once before bed. For those at higher risk, it is beneficial to floss after each meal. It is also important to floss before you brush once daily to loosen any food particles or bacteria between your teeth.
How often should I see my dentist for prevention of gingivitis and periodontitis?
For most adults, seeing your dentist once or twice a year for regular teeth cleaning can help prevent not only periodontitis but a myriad of other dental issues. Some patients who are at higher risk for periodontitis may need more frequent teeth cleaning. Consult with your dentist to find out what is appropriate for your risk level.
gum disease and other health implications
Bacteria associated with gum disease will make its way from the mouth into the bloodstream, which can cause some serious other health problems for susceptible populations. Recent CDC research has found evidence linking gum disease with heart disease, stroke, respiratory disease, premature birth for pregnant women, and diabetes.
Call Us at (303) 671-0305 to learn more about periodontal disease.


